Introduction
Chimeric antigen receptor (CAR) T-cell therapy targeting CD19 has demonstrated promising efficacy in patients with relapsed and refractory (R/R) B-cell acute lymphoblastic leukemia (B-ALL). However, relapse after CART remains a major issue. Here, we analyzed the factors related to long-term efficacy, including overall survival (OS), leukemia-free survival (LFS) and cumulative relapse rate (CRR), following CAR-T therapy in 231 R/R B-ALL patients who achieved complete remission (CR) within one month after CAR T-cell therapy.
Patients and Methods
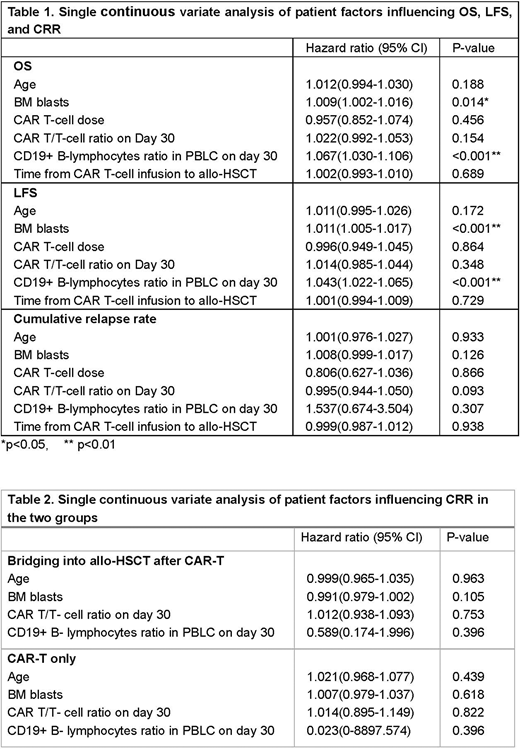
From April 2017 to March 2019, 254 patients with R/R B-ALL were enrolled onto one of five different clinical trials (NCT03173417; ChiCTR-ONC-17012829; NCT02546739; ChiCTR1800016541; and NCT03671460) at our center and received a second generation CD19+ CAR T-cell infusion. The median infused CAR T-cell dose was 3×105/kg (range: 0.2-10×105/kg). The CAR-T/T-cell ratio and the CD19+ B lymphocyte percentage in PBLC samples from 159 of the patients were analyzed using flow cytometry on day 0, 4, 7, 11, 14, 21, and 30 following CAR T-cell infusion. We performed single continuous variate factors analysis on the influence of the CAR-T/T-cell ratio and the percentage of CD19 + B-lymphocytes in day 30 post-infusion PBLC samples on the OS, LFS, and CRR. We also analyzed the impact of patient age, BM blast count, CAR-T-cell dose, and the interval time between CAR-T-cell therapy and consolidation allogeneic hematopoietic stem cell transplantation (allo-HSCT) on OS and LFS.
Results
Among 254 patients, 231 cases achieved CR within one month after CART therapy. A total of 211 CR patients had long-term follow-up of more than 30 days with a median follow-up of 12 months (1 to 29 months). On day 30 post CAR T-cell infusion, the median CAR-T/T-cell ratio in PBLC samples was 0.51% (range: 0%-44.8%), with 59 of 169 patients (34.9%) having a CAR-T/T-cell ratio of ≥1% and 85 of 169 patients (50.3%) with a CAR-T/T-cell ratio of ≥0.5%. The median percentage of CD19+ B lymphocytes in PBLC on day 30 was 0.0% (range: 0.0%-9.4%), of which 157 of 169 patients (92.9%) had <0.5% CD19+ B-cell lymphocytes, and 137 of 169 patients (81.1%) had <0.1% CD19+ B lymphocytes on day 30.
Using a single continuous variate factors analysis, we found that increasing BM blasts and percentage of CD19+ B-lymphocytes in PBLC samples on day 30 correlated with a worse OS and LFS (Table 1). BM blasts of ≥70% were statistically significantly correlated with a worse OS and LFS when compared to BM blasts of <70% (2-year OS of 52.6% vs. 65.0%, p=0.041; 2-year LFS of 43.3% vs. 58.6%, p=0.023). Unlike the BM blast data, for the CD19+ B-lymphocytes percentage in PBLC samples on day 30, we not identify a cut-off threshold. The CAR-T/T-cell ratio in PBLC samples on day 30 had no influence on OS or LFS. Unfortunately, the CAR-T/T- cell ratio and CD19+ B-lymphocyte percentage data beyond day 30 following CAR T-cell therapy was lacking for most patients and further analysis could not be performed to understand the impact of these factors on long-term survival. In our analysis, CAR T-cell dose, the interval time between CAR T-cell infusion and allo-HSCT did not significantly correlate with OS, LFS, or relapse.
The remaining 184 patients in CR received a consolidation allo-HSCT after a median interval time of 67 days post CAR T-cell therapy (range: 30-334 days). Thirty-two of these patients (17%) relapsed with a median time to relapse of 221 days (57-490 days). The remaining 27 patients received CAR T-cell therapy only and 11 (41%) relapsed with a median time to relapse of 100 days (53-398 days). None of the four factors above had an influence on the CRR in either the bridging into allo-HSCT group or the CAR-T only group (Table 2).
Conclusions
Using a single continuous variate factors analysis, we found that a high BM blast count and the percentage of CD19+ B-lymphocytes in PBLC samples from R/R ALL patients on day 30 predicted a worse OS and LFS while age, the CAR-T/T-cell ratio on day 30, CAR-T cell dose, and the interval time between CAR-T cell infusion and allo-HSCT had no clear impact on long-term outcomes.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal